Introduction
Guillain-Barre Syndrome (GBS) and Myasthenia Gravis (MG) are common causes of acute weakness. About 25% of these patients may develop respiratory failure requiring intubation, so a major concern is determining who requires ICU-level monitoring and whether intubation should be performed. Ideally it would be possible to predict with 100% accuracy which patients would require intubation, allowing pre-emptive elective intubation. In reality such prediction is impossible, so we are often forced to carefully observe patients in the ICU until they declare themselves.
Foreword: Some comments on bedside pulmonary function tests (PFTs)
Bedside PFTs are not the comprehensive set of tests obtained in the outpatient clinic, but rather some very basic tests performed at the bedside by a respiratory therapist. These consist of:
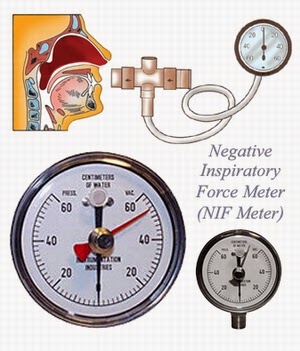
- MIP = Maximal Inspiratory Pressure. This is the greatest negative pressure the patient can generate, often also referred to as the NIF (Negative Inspiratory Force). It is measured asking patients to inhale as hard as they can with measurement of the negative pressure that they generate using a pressure gauge (image above). This is a measurement of the strength of the inspiratory muscles, primarily the diaphragm.
- MEP = Maximal Expiratory Pressure. This is the opposite of the MIP, specifically the maximal positive pressure the patient can generate. It is measured by asking patients to exhale as hard as they can, and measuring the positive pressure. This is a measurement of expiratory muscle strength, which may correlate clinically with ability to cough and clear secretions.
- FVC = Forced vital capacity. This is the largest volume of gas that a patient can exhale. Patients are asked to take a full breath in and then exhale maximally, with measurement of the exhaled volume. FVC reflects a global measurement of the patient's ventilatory ability, which takes into account inspiratory and expiratory muscle strength as well as pulmonary compliance.
Pearl #1: Do not intubate a patient solely because of poor PFTs
It is widely believed that patients with GBS and MG who have severely impaired pulmonary function should be intubated pre-emptively. A commonly cited rule for GBS patients is the 20-30-40 Rule: intubation is indicated if the FVC falls below 20 ml/kg, the MIP is less than 30 cm water, or the MEP is less than 40 cm water. This is a myth. Poor PFTs correlate with risk of respiratory failure, but are not highly specific for predicting intubation. Unfortunately, PFTs were rapidly incorporated into patient care before being adequately evaluated, leading to a spiral of circular logic which extends from the 1980s until today:
The 20-30-40 rule is generally attributed to Lawn 2011. This was a retrospective study of 114 patients with GBS admitted to intensive care at the Mayo Clinic between 1976-1996. Significant correlations were found between poor pulmonary function tests and respiratory failure, but no single test (FVC, MIP, or MEP) predicted intubation well (table below). Therefore, these authors proposed that patients meeting any of these three criteria should be monitored in the ICU and considered for elective intubation. This rule was proposed in the conclusions section of the paper, but at no point in the manuscript was the sensitivity or specificity of the combined rule actually evaluated. The closest they came to testing this was performing multivariable analysis which revealed that only FVC was an independent predictor of respiratory failure, thus challenging their own rule by demonstrating that MIP and MEP don't actually add independent information. The 20-30-40 rule has been propagated in the literature for 14 years despite lack of clear evidence supporting it.
 |
Original data on which the 20-30-40 rule for GBS was based (from Lawn 2011). Note the poor degree of separation between patient groups based on Pimax (a.k.a. MIP) and Pemax (a.k.a. MEP). Based on the vital capacity data above, the specificity of the 30-40-50 rule must be 83% or lower (given that 17% of patients who didn't require ventilation had a vital capacity below 20 ml/kg). |
Pulmonary function tests are even less useful in MG because this disease has a less predictable course. Initial pulmonary function tests are very poorly predictive of the need for intubation (Rieder 1995, Thieben 2005). Although some critical care textbooks acknowledge this uncertainty, others recommend elective intubation based on FVC and MIP cutoffs borrowed from GBS (e.g., one prominent source recommends elective intubation when the FVC falls under 15-20 ml/kg or the MIP is under 25-30 cm, a truncated version of the 20-30-40 rule for GBS). These cutoffs have not been validated for GBS, and thus should not be extrapolated to another disease.
As with any critically ill patient, the decision to intubate should be based primarily on clinical assessment at the bedside. Important elements include work of breathing, respiratory rate, oxygenation variables, and trends in these values. Other indications for intubation would include bulbar dysfunction with an inability to handle secretions and protect the airway. Significant hypoxemia would suggest either ongoing aspiration or atelectasis, either of which would be very concerning. The overall tempo of the illness and clinical context, including trends in pulmonary function, provides some additional information.
Since pulmonary function tests are poorly specific for predicting respiratory failure, pre-emptive intubation based solely on pulmonary function tests may lead to unnecessary intubations and iatrogenic harm. A safer approach to patients with poor pulmonary function who do not clinically require intubation is close ICU-level observation with intubation only if clinically indicated. It is also possible that noninvasive ventilation could be used to preventthese patients from failing (more below).
Pearl #2: Don't check the MIP or MEP
FVC is arguably the best single test of ventilatory capability, since it integrates inspiratory and expiratory muscle strength as well as pulmonary compliance. It is also the most reproducible test over time. Therefore it should come as no surprise that nearly all studies have focused exclusively on the FVC in predicting respiratory failure, completely ignoring the MIP and MEP (e.g., Sunderrajan 1985, Chevrolet 1991, Sharshar 2003, Durand 2006, Kanikannan 2014).
MIP and MEP do not add additional information to what is provided by the FVC. In multivariable models, Lawn 2001 found that neither MIP nor MEP added statistically independent information to the FVC. Both MIP and MEP had little ability to identify patients progressing to ventilatory failure, with substantial overlap between values obtained in patients who did and did not require intubation (table above). Prigent 2012 found a linear relationship between VC and MIP, with MIP failing to add information to FVC. Any impairment in inspiratory or expiratory muscle strength measured by the MIP and MEP will be physiologically integrated into the FVC, so there appears to be little added value in measuring the MIP and MEP separately.
MIP and MEP are more effort-dependent and less reproducible than FVC, so when tracking serial PFTs adding the MIP and MEP adds significant noise. Some patients with bulbar involvement may have difficulty sealing their lips around the mouthpiece, leading to inaccurate MIP and MEP measurements (1). Finally, it must be kept in mind that when the MIP and MEP are performed urgently in the emergency department or ICU, this will be less rigorous and methodical than when the same tests are performed in a formal outpatient PFT laboratory. More information doesn't guarantee more accurate information.
Pearl #3: Don't assume respiratory failure is due to respiratory muscle weakness
Patients who have been labeled with GBS or MG are susceptible to anchoring bias: there is a tendency to assume that any respiratory problem encountered must be due to their neuromuscular weakness. Once we were told that a patient transferred to Genius General Hospital with MG and respiratory failure required urgent intubation. Indeed, the patient arrived quite dyspneic and hypoxemic. Bedside ultrasonography showed a large right-sided pleural effusion, and further evaluation revealed that the patient had congestive heart failure with severe volume overload. Therapeutic thoracentesis and heart failure management caused immediate improvement, avoiding the need for intubation. Although the patient may have known respiratory muscle weakness, don't forget to look for other problems as well. When in doubt, unholster the triple-barreled shotgun:
Pearl #4: Consider early pre-emptive respiratory support with BiPAP or high-flow nasal cannula.
The pulmonary outcome of a patient with MG or GBS will often depend on the balance between the respiratory muscle strength and the work of breathing. If the scale is tipping slightly in the wrong direction, the patient will gradually fatigue and eventually fail. For patients who are hanging in the balance, even a small reduction in the work of breathing could be critical. However, in order for this to succeed respiratory support must be initiated early, well in advance of respiratory exhaustion.
There is little high-quality evidence about BiPAP in this situation. Three retrospective case series describe the use of BiPAP in myasthenia gravis, with avoidance of intubation in ~60% of cases (Rabinstein 2002, Wu 2009, Seneviratne 2008). Of note, Rabinstein reported avoiding intubation in 7/11 cases of myasthenia gravis, despite very low baseline FVC values (all patients had FVC <10 ml/kg). These series noted increased failure rates among patients with significant baseline hypercapnia, suggesting that such patients may have progressed to a point of respiratory fatigue that cannot be rescued by BiPAP. Evidence with Guillian-Barre syndrome is more sparse, with two case reports of BiPAP failure and one case report of success (Pearse 2003, Wijdicks 2006).
There is no clinical evidence with high-flow nasal cannula. High-flow nasal cannula can reduce anatomic dead space causing a reduction in the work of breathing as discussed here. Although high-flow nasal cannula provides less ventilatory support than BiPAP, it may be used in patients who have contraindications to BiPAP or cannot tolerate the BiPAP mask.
In absence of solid evidence, a cautious trial-and-error approach may be reasonable (above). The best metric to gauge success of these interventions may be improved patient comfort with reduced respiratory rate. One advantage of BiPAP and high-flow nasal cannula is that it is easy to trial them, and they may be immediately discontinued if they are not helping.
One risk of using BiPAP or high-flow nasal cannula is that if inadequately monitored they theoretically could mask progressive respiratory failure until the patient was extremely unstable. Therefore, this should be performed with ICU-level monitoring and close attention for any signs of clinical deterioration or worsening hypoxemia. Patients with GBS and MG typically should not have substantial hypoxemia, so escalating oxygen requirement suggests a complication such as mucus plugging, atelectasis, or aspiration (which would usually indicate the need for intubation).
Pearl #5: Try not to chase dysautonomia in GBS. However, be prepared to handle it in the peri-intubation period.
Patients with GBS may have dysautonomia with hemodynamic lability. One risk involved in this situation is that if the "highs" are over-treated, this may exacerbate the "lows." That is, if hypertension or tachycardia is treated (for example, with a beta-blocker), then the patient could subsequently have an episode of severe hypotension and bradycardia. It is often best to avoid treating these fluctuations if possible. If treatment is needed, a very short-acting agent may be safest so that it can be discontinued rapidly if needed. Any factors aggravating hemodynamic swings (e.g. untreated pain, underlying hypovolemia) should be corrected.
Dysautonomia is a particular concern in the peri-intubation period, as it may combine with hemodynamic fluctuations following intubation, amplifying the risk of hypotension. These patients are often volume depleted due to poor oral intake, so it is sensible to assess volume status prior to intubation (e.g. with ultrasonography) and resuscitate to a euvolemic state. Peri-intubation bradycardia is mediated by the parasympathetic nervous system, so atropine is a logical first-line treatment for this and should be close at hand.
- The only bedside pulmonary function test which is useful is the forced vital capacity (FVC).
- Patients with a FVC < 20 ml/kg are at risk for respiratory failure and should receive ICU-level monitoring.
- Intubation is typically required when the FVC falls below 10-15 ml/kg. However, the decision to intubate is a clinical decision based primarily on ability to protect the airway, work of breathing, vital signs, overall appearance, and trajectory.
- For patients who are dyspneic but don't require intubation, consider trialing BiPAP or high-flow nasal cannula to see if this may improve their comfort and reduce the work of breathing.
- Patients with GBS may have dysautonomia with wide fluctuations in blood pressure. Avoid treating hypertension if possible, as this may exacerbate subsequent episodes of hypotension.
Notes
(1) In the spirit of full disclosure, I underwent a complete set of pulmonary function tests during my training, for educational purposes. My MEP was statistically low due to difficulty with the mask seal. I've held a grudge against the MEP ever since. Seriously, though - if you've never had PFTs performed on yourself this is a very informative exercise. It will demonstrate how effort-dependent these tests are, and how some maneuvers (especially the MIP) are a bit fatiguing and uncomfortable.
Image Credits:
http://library.westprime.com/store/index.cfm?do=DetailProduct&productid=2436&categoryid=409&ParentID=5&categoryname=Negative%20Inspiratory%20Force%20Meter
http://etc.usf.edu/clipart/41800/41848/balance_41848.htm
http://rsolosky.com/wp-content/uploads/2013/06/speeding-bullet-2.jpg